Iron deficiency leads to inadequate stores for heme incorporation, slowing erythrocyte production and leading to a microcytic anemia.
—Causes—
Chronic Blood Loss
Chronic blood loss leads to iron deficiency as iron is lost with the red blood cells instead of being recycled by the body. For women, prolonged or heavy periods can deplete the iron stores and cause anemia. Other causes include gastrointestinal bleeding, hemorrhoids, hematuria, etc. Any conditions which cause intravascular hemolysis or prolonged bleeding can lead to iron deficiency and consequently, anemia.
Increased Demand
Iron deficiency may occur when there is an increased need for iron that is not being met, such as in infants and children where there is a lot of growth. Additionally, pregnant and nursing mothers need more iron to provide for their developing baby.
Inadequate Intake
Poor diet can lead to iron deficiency as not enough iron is brought in to replenish stores. Heme iron is found in meat, fish, and poultry and is more readily absorbed than the non-heme iron found in legumes and dark leafy greens. Iron deficiency due to inadequate intake is far less common in developed countries, as many foods are fortified with iron. Strict vegetarians may still become deficient however, as their diet consists of non-heme iron.
Malabsorption
Before most iron can be used by the body, it must first be properly broken down from ferric iron to ferrous iron in the stomach. Medications or conditions that decrease stomach acidity can inhibit this breakdown, causing less iron to be absorbed. Since most iron absorption takes place in the small intestine, conditions like Celiac or Crohn’s disease can also cause iron insufficiency as not enough iron is absorbed.
—Stages—
Stage I
The first stage of iron deficiency does not present with any symptoms, as iron stores are sufficient to continue normal erythrocyte development. Ferritin levels decrease as the iron stores are used without being sufficiently replenished. With no symptoms however, ferritin is not likely to be tested.
Stage II
The second stage of iron deficiency occurs when iron stores are depleted and can no longer compensate for the insufficiency.
Ferritin and iron levels in the serum are decreased. Transferrin increases in an attempt to bind more iron. Total Iron Binding Capacity (TIBC) is often used to indirectly measure transferrin since they are directly proportional to each other.
Hemoglobin content in erythrocytes begin to decrease as newer cells are made with less iron available. These newer cells will have decreased mean cell volume (MCV) as they take longer to mature. Since the lifespan of erythrocytes is about 120 days, the majority of circulating cells are still from when iron levels were normal. Thus, overall hemoglobin is just starting to decrease. Red cell distribution width (RDW) will also start increasing as more microcytes are formed.
Stage III
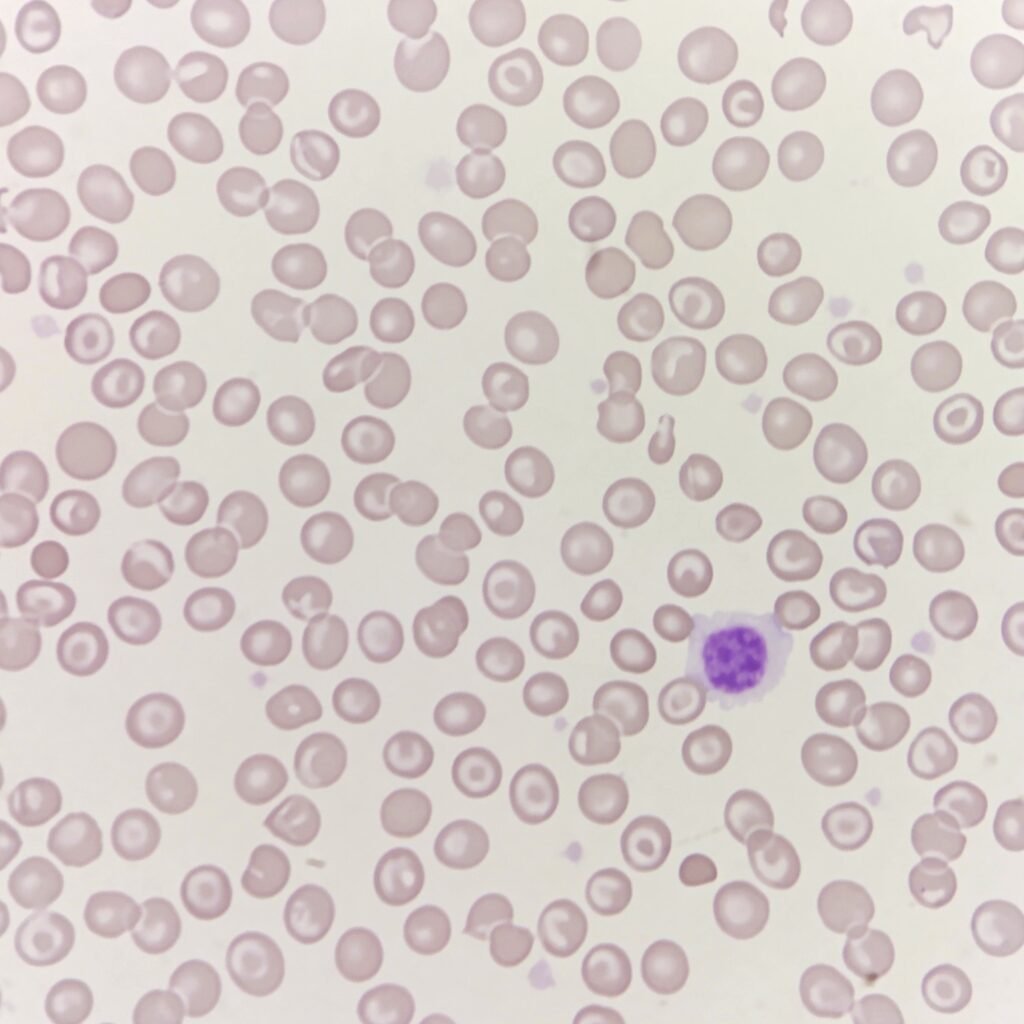
In the third stage, iron deficiency has progressed to a hypochromic, microcytic anemia.
——
References
- Iron – Medicine LibreTexts
- 18.3 Erythrocytes – Anatomy & Physiology 2e
- Iron deficiency anemia – Symptoms & causes – Mayo Clinic
- Anemia – Iron-Deficiency Anemia | NHLBI, NIH
- Iron deficiency anemia: MedlinePlus Medical Encyclopedia
- 12.7: Iron – Medicine LibreTexts
- 4.1: Iron Deficiency Anemia (IDA) – Medicine LibreTexts
